State of the Union: Weight Loss Surgery and Non-Surgical Procedures in 2024
Explore the evolving landscape of weight loss surgery and non-surgical procedures. Discover trends and the number of weight loss procedures performed annually.

Co-founder, CEO
There’s a lot of hype around GLP1 medications such as Ozempic, Wegovy, and Zepbound. However, weight loss procedures, both surgical and non-surgical, continue to be a rapidly growing area for those seeking one-time interventions without the long-term use of medications. From the outside, it might seem like weight loss procedures have remained static, but the reality is far from it. With numerous surgical and non-surgical options available, the landscape is constantly evolving. Let’s dive into the numbers and see what they reveal!
We’ve published many articles and studies on the clinical implications of weight loss procedures including this treatment comparison table. In this article, I hope to do something different and tackle the topic from an industry trend standpoint. I hope this overview is helpful for those seeking weight loss interventions, as well as practitioners and business folks looking to understand the entire weight loss procedure space better. Let’s dive into the numbers and see what they reveal!
Fast-Changing and Dynamic Weight Loss Procedure Landscape
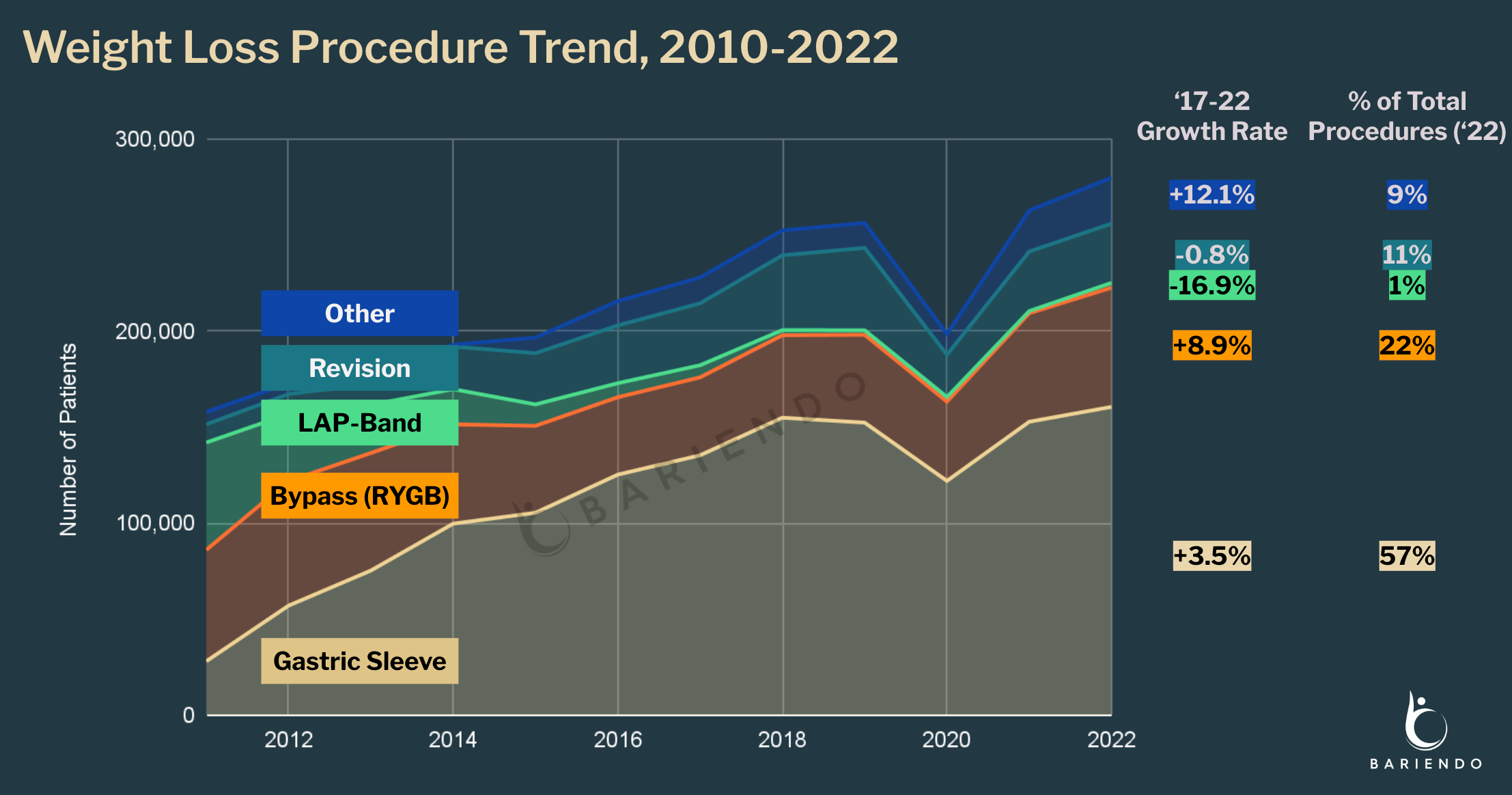
The American Society for Metabolic and Bariatric Surgery (ASMBS) reported that 280,000 Americans underwent weight loss procedures in the most recent year with available data. This represents a 4.2% annual growth over the past five years, with approximately 1 in 100 individuals with Class III obesity (BMI over 40) opting for bariatric surgery annually.
The top three weight loss procedures by volume are:
-
Gastric Sleeve (Sleeve Gastrectomy) is the most popular weight loss surgery in the U.S., accounting for 57% of procedures performed in 2022. A total of 160,609 patients underwent this procedure.
-
Gastric Bypass (RYGB) follows as the second most common option, representing 22% of surgeries with 62,097 patients.
-
Revision Surgeries, performed to correct previous bariatric procedures, account for 10% of all bariatric procedures with 30,894 cases in 2022.
Interestingly, the “Other” category of weight loss procedures is the fastest-growing group, with a 12.1% annual growth rate. This highlights the dynamism of the field, with many new procedures being developed and authorized even in recent years.
A Closer Look at Best-Known Weight Loss Surgery: Sleeve, Bypass, LAP-Band
When discussing bariatric surgeries, the most well-known are gastric sleeve, gastric bypass, and LAP-Band. Let’s examine these in more detail.
Gastric Sleeve (Sleeve Gastrectomy or SG) involves removing a portion of the stomach to create a smaller, sleeve-shaped stomach. This surgery delivers 23% weight loss, and usually requires hospitalization.
Gastric Bypass (Roux-en-Y) involves creating a small pouch from the original stomach and connecting it directly to the small intestine, bypassing most of the stomach. It delivers the highest weight loss rate (around 30%) but is more invasive and has a longer recovery time.
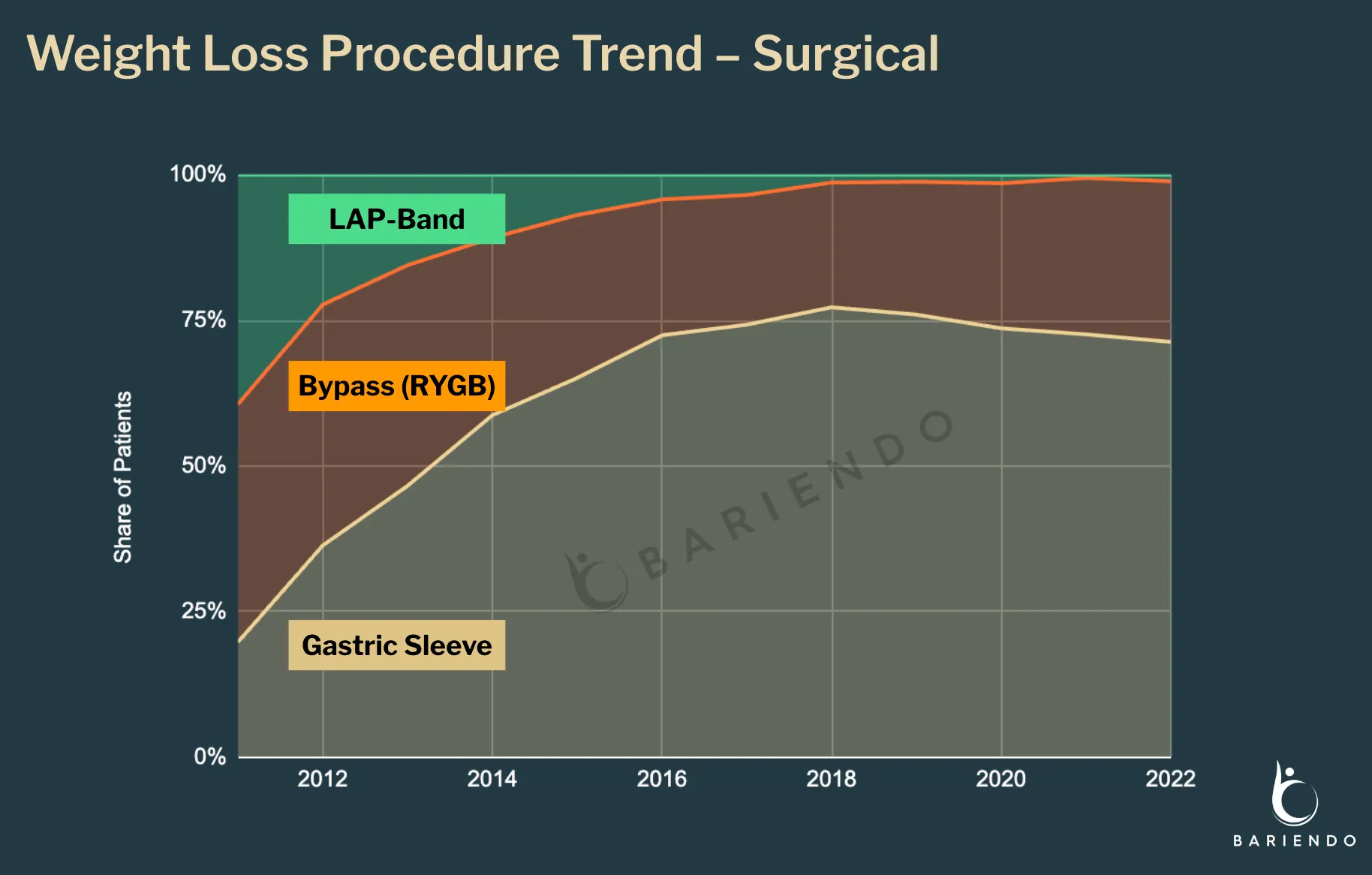
LAP-Band involves placing an adjustable band around the upper part of the stomach. The procedure results in approximately 15% weight loss. LAP-Band used to be one of the most popular bariatric surgical procedures, but has fallen out of favor due to high rates of re-operations, lower weight loss, and inadequate follow-up care. By 2019, it accounted for less than 1% of weight loss surgeries.
More than ten years ago, gastric bypass used to be the most popular form of bariatric surgery. Gastric sleeve has surpassed gastric bypass as the most popular bariatric surgery by 2013. This shift reflects a broader industry trend towards less invasive procedures with lower complication rates. Gastric sleeve typically has a complication rate of 12-15% compared to 18% for gastric bypass.
While gastric sleeve has gained popularity due to its less invasive nature, gastric bypass remains the recommended option for individuals seeking significant weight loss (30% or more) and those with related health conditions like diabetes. It consistently delivers the highest weight loss results among common bariatric procedures.
It’s important to note that recent data suggests a link between gastric sleeve and acid reflux, which may increase the risk of esophageal cancer. This factor has contributed to a slower growth rate for gastric sleeve procedures in recent years.
The Future of Weight Loss Procedures: Endoscopic and Non-Surgical
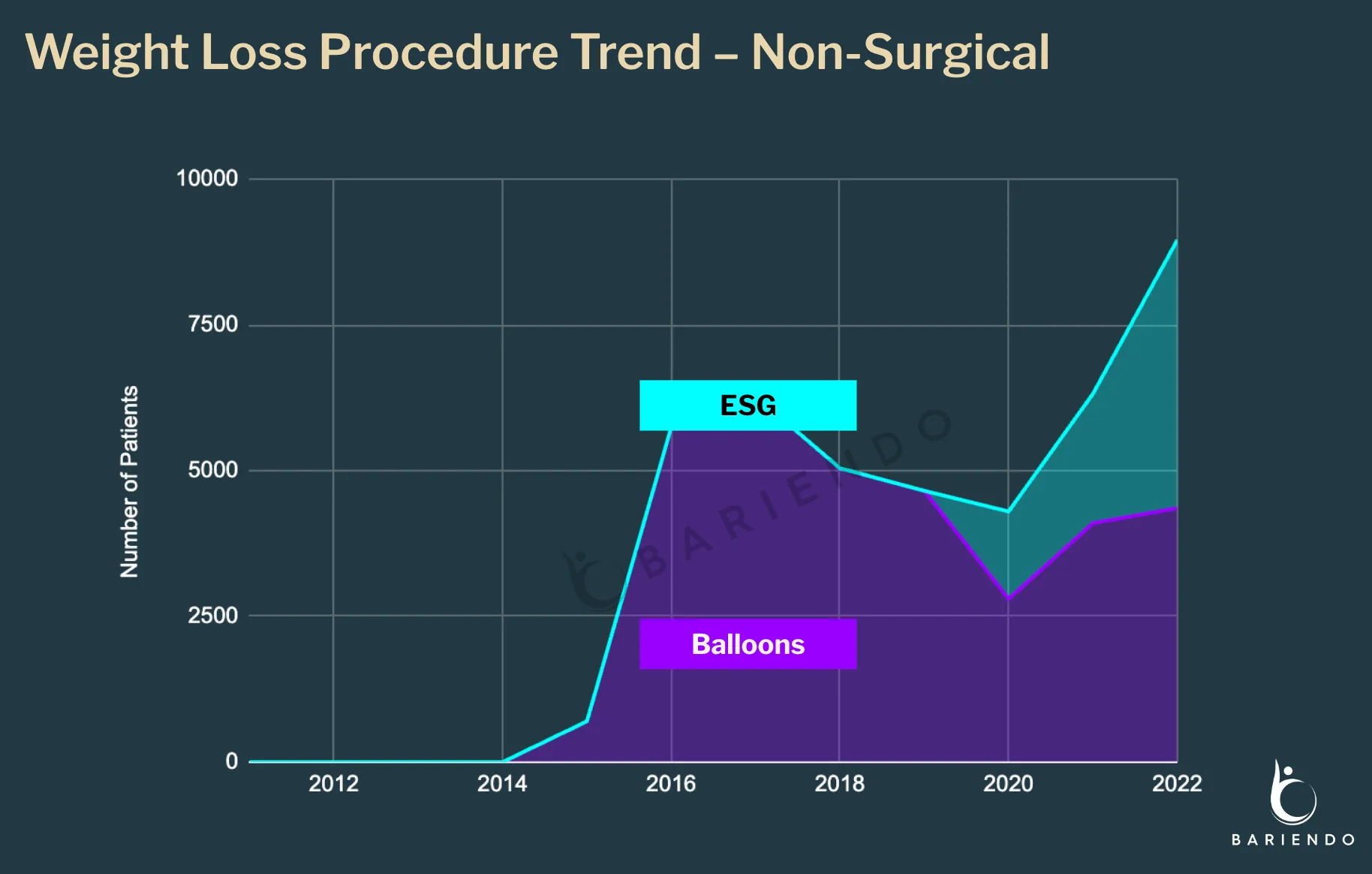
Just as the gastric sleeve has dominated the weight loss surgery space, a new class of weight loss procedures is emerging: non-surgical endoscopic weight loss procedures. Building upon the minimally invasive advancements of laparoscopic surgery, endoscopy offers an even less invasive approach. Performed through the mouth without incisions, these procedures significantly reduce recovery time and risks.
The two broad categories of non-surgical, endoscopic weight loss procedures are gastric balloon (IGB) and endoscopic sleeve gastroplasty (ESG). Gastric balloon involves temporarily placing a balloon in the stomach to occupy space and reduce food intake. Endoscopic Sleeve Gastroplasty (ESG) involves folding and suturing the stomach from the inside to reduce its size without any surgery.
ESG may go by different names in the market, including Bariendo’s ESG Stomach Tightening. These different versions of ESG differ slightly in the number and pattern of sutures used but are all broadly categorized as ESG.
The move from laparoscopic to endoscopic procedures has significantly reduced recovery times and complication rates. Recovery time has decreased from 2-4 weeks to 1-3 days, and complication rates have dropped from 12-18% to below 1%. Additionally, these procedures are now approved for individuals with a BMI over 27, expanding access to more people. Unlike laparoscopic gastric sleeve, which leaves small scars on the abdomen, ESG leaves no scars.
Dr. Christopher Thompson of Harvard Medical School and co-founder of Bariendo first performed ESG in a human in 2012. Since its FDA authorization in July 2022, ESG has become the fastest-growing weight loss procedure, tripling in number from 2020 to 2022, with an estimated 4,600 patients undergoing the procedure in 2022. ASMBS’s ESG numbers are likely significantly underreported due to the recent implementation of ESG reporting.
However, ESG might still be relatively small in the overall landscape due to its recent FDA approval and a shortage of official training programs. Currently, there are only two advanced fellowship programs in the country that include ESG, one of which is at Brigham and Women’s Hospital run by Dr. Pichamol Jirapinyo.
But What About Tummy Tuck or Liposuction?
Tummy tuck (Abdominoplasty) and liposuction are often confused with weight loss procedures, but they are cosmetic body contouring surgeries, not intended for significant weight loss.
Tummy tuck involves removing excess skin and fat from the abdomen and tightening the abdominal muscles, whereas liposuction focuses on removing fat from specific areas of the body using suction.
These procedures can enhance body contour but typically do not result in significant weight loss. The ideal candidate for tummy tuck surgery is someone who is at or near their normal weight, active, and healthy but has concerns about a protruding abdomen or sagging, loose skin on their stomach. Both of these surgeries are not recommended for individuals with a BMI over 30.
According to the American Society of Plastic Surgeons, more than 700,000 people undergo tummy tuck and liposuction procedures each year in the United States.
What is the Clinical Future of Weight Loss?
In recent years, there has been increasing recognition that obesity is a medical condition rather than lifestyle and willpower issues. The trend has been driven by the approvals of multiple GLP1 agonists such as Ozempic, Wegovy, Zepbound, and Mounjaro. This has led to a surge in clinical weight loss interventions in recent years.
Medical interventions are never one-size-fits-all, and multiple treatment methods coexist as tools in physicians’ toolboxes. Obesity specialists generally agree that the future of clinical weight loss interventions will likely involve three tiers:
-
Anti-Obesity Medications (GLP1 Agonists): The least invasive, but requiring continuous use.
-
Non-Surgical Endoscopic Procedures (ESG): Mid-tier solutions that are outpatient, minimally invasive, and offer durable results with lower complication rates.
-
Bariatric Surgeries (Gastric Sleeve and Gastric Bypass): The most invasive, reserved for those needing significant weight loss.
It’s an exciting time in the field of obesity interventions, with many new innovations on the horizon – both in medications and procedures. On the medication side, research focuses on improving drug delivery, transitioning from injectables to oral forms, and targeting receptors beyond GLP1s. However, the main challenge remains weight rebound after discontinuation and managing side effects.
For weight loss procedures, research aims to develop new techniques for better, more durable results and to introduce new medical devices that make ESG-like procedures more affordable and accessible, as current devices often require specialized skills and dexterity. My Bariendo co-founders, Dr. Christopher Thompson and Dr. Pichamol Jirapinyo of Harvard Medical School, are leading major studies to continue to refine non-surgical weight loss procedures and devices.
With almost half of America affected by obesity, we now have the clinical tools to reverse this pandemic. These advancements are crucial in addressing this significant health issue and helping millions achieve better health.