Obesity Primer for the Practicing Gastroenterologist
A guide for gastroenterologists on assessing and managing obesity, covering definitions, related GI conditions, evaluations, treatments, and complications.


Co-founder, SVP of Longitudinal Care
This post provides an updated summary of the academic paper “Obesity Primer for the Practicing Gastroenterologist” by our cofounders, Dr. Pichamol Jirapinyo and Dr. Christopher C. Thompson.
Introduction
Obesity is a pandemic, affecting over 650 million adults, which is about 13% of the world’s population. In the United States, this number is even higher, with 42.4% of adults classified as having obesity. Recognized as a chronic disease by the American Medical Association, obesity is defined by the Obesity Medicine Association as a condition involving increased body fat leading to adverse health effects. Traditionally, obesity is measured using a Body Mass Index (BMI), with categories ranging from class I (BMI 30–34.9 kg/m²) to class III (BMI ≥40 kg/m²). However, BMI has limitations, especially among the elderly and muscular individuals. Waist circumference and body fat percentage are alternative measures, with specific cutoffs indicating central obesity, which is linked to higher health risks. Understanding these definitions and measurements is crucial for gastroenterologists, who will see an increasing number of patients with obesity due to the pandemic nature of this disease.
Obesity-Related Gastrointestinal Conditions
Obesity is associated with several gastrointestinal (GI) conditions, leading to higher incidence rates and more severe manifestations. Some key conditions include:
-
Esophageal Disorders: Obesity increases the risk of gastroesophageal reflux disease (GERD), esophagitis, and esophageal adenocarcinoma (a type of esophageal cancer).
-
Liver Diseases: Fatty liver is highly prevalent among patients with obesity. Additionally, obesity accelerates the progression of liver conditions.
-
Pancreatic and Biliary Diseases: Obesity is linked to pancreatitis and gallbladder diseases.
Recognizing these associations helps gastroenterologists in early diagnosis and management of obesity, potentially reducing the severity and prevalence of these GI conditions.
Evaluating Obesity
Initial Assessment
The initial evaluation includes assessing the patient’s readiness to change their health behaviors using the “Stages of Change” model, which ranges from precontemplation (unaware of the need for change) to maintenance (sustaining new behaviors for over six months). Techniques like motivational interviewing can assist in moving patients through these stages.
Medical Evaluation
A comprehensive medical history and physical examination should include weight-focused assessments, medication history reviews, and laboratory tests. Physical signs of obesity-related conditions, such as insulin resistance or polycystic ovarian syndrome, should be assessed.
Lifestyle Evaluation
Understanding dietary habits through tools like a 24-hour diet recall, and evaluating physical activity levels are essential. Total energy expenditure, which includes resting energy expenditure, the thermic effect of meals, and energy expenditure from physical activity, should be assessed to understand the patient’s caloric needs and deficits.
Psychological Evaluation
Assessing for psychiatric conditions like anxiety, depression, and eating disorders is crucial, as these can affect weight and eating behaviors. Tools like the Eating Disorder Examination Questionnaire can help in identifying these issues.
Endoscopic Evaluation
Endoscopy may be needed for certain patients, especially those undergoing bariatric surgery. This helps in identifying conditions like hiatal hernia, esophagitis, and other abnormalities that may affect surgical outcomes.
Managing Obesity
Lifestyle Modification
First-line treatment involves lifestyle changes focusing on diet, exercise, and behavioral therapy. Effective dietary interventions can range from low-calorie diets to macronutrient-focused plans like low-carb or high-protein diets. Regular physical activity, including aerobic exercises and resistance training, is crucial. Behavioral therapy components, such as self-monitoring and cognitive restructuring, help in maintaining these lifestyle changes in the long term.
Pharmacotherapy
Weight-loss medications may be considered for patients who do not respond to lifestyle changes and have a BMI of ≥30 or ≥27 with at least one comorbidity. Medications include phentermine, orlistat, phentermine/topiramate, naltrexone/bupropion, liraglutide, semaglutide, and tirzepatide. Each medication has specific indications, efficacy, and potential side effects, which need to be discussed with patients before initiation.
Bariatric Endoscopy
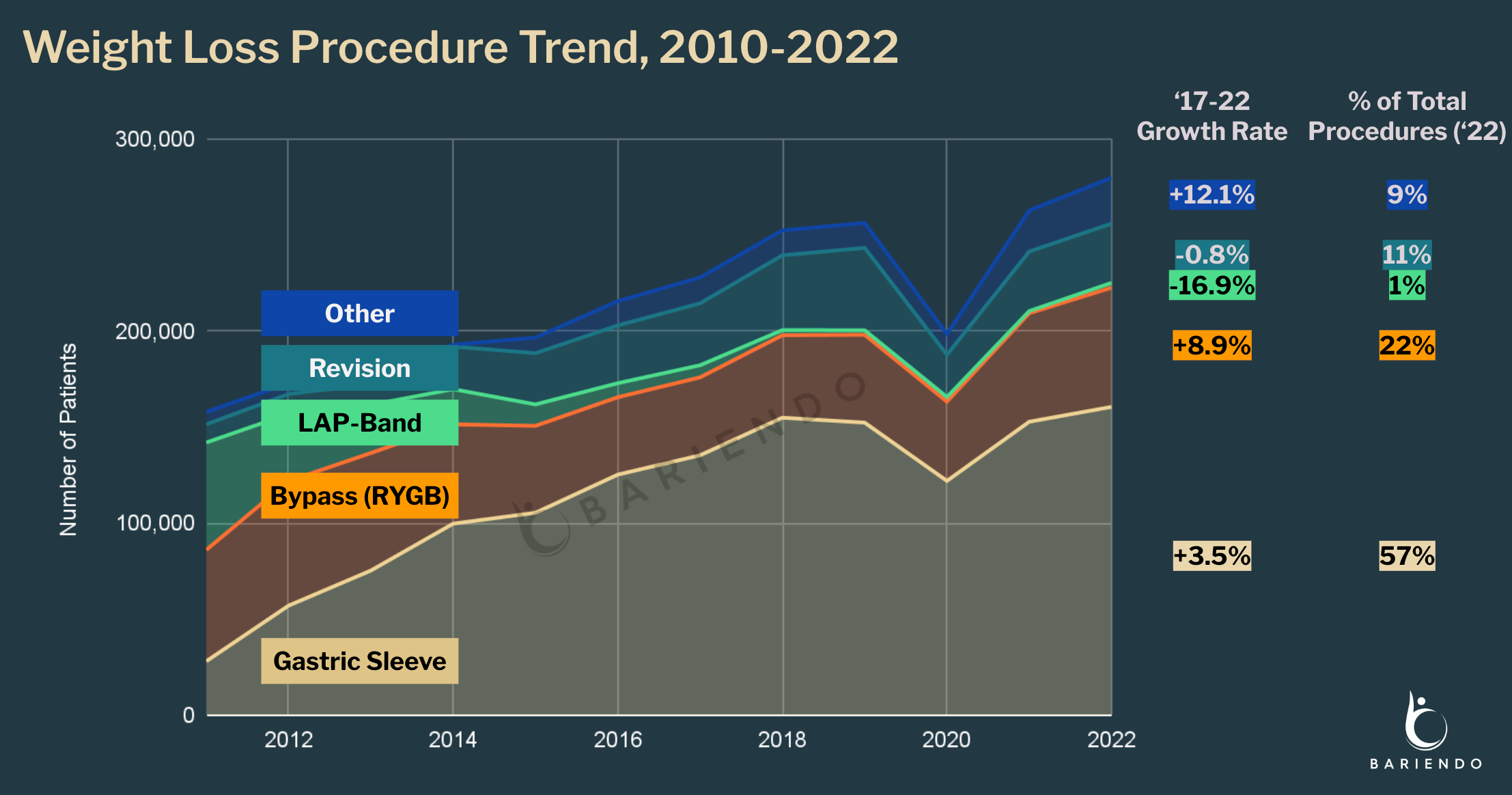
Bariatric endoscopic interventions can be categorized into gastric and small bowel procedures. Gastric interventions, like intragastric balloons and endoscopic sleeve gastroplasty (ESG), primarily induce weight loss. Small bowel interventions mainly affect metabolic conditions, such as diabetes and fatty liver. These procedures are being performed increasingly, especially for patients not eligible for surgery.
Bariatric Surgery
Bariatric surgery is considered for patients with a BMI of ≥40 or ≥35 with at least one comorbidity. Common surgical procedures include sleeve gastrectomy and Roux-en-Y gastric bypass, each with specific outcomes and complication profiles. Understanding these procedures helps in managing patients pre- and post-surgery.
Managing Complications of Bariatric Surgeries
Gastroenterologists must be familiar with common complications of bariatric surgeries, such as leaks, stenosis (narrowing of the GI lumen), and nutritional deficiencies. Early identification and appropriate management strategies, which may include endoscopic interventions, are essential for improving patient outcomes.
Developing Expertise in Obesity Medicine and Bariatric Endoscopy
Gastroenterologists can enhance their expertise in obesity medicine and bariatric endoscopy through specialized training and certification, such as the American Board of Obesity Medicine and Bariatric Endoscopy Fellowship. Establishing a multidisciplinary team and a supportive clinic environment is crucial for effective obesity management.
Conclusion
Gastroenterologists play a vital role in managing obesity and its related GI conditions. With the increasing prevalence of obesity, it is essential to integrate comprehensive assessment and management strategies into clinical practice to address this growing health concern effectively.